Cancer, the uncontrolled abnormal growth of cells, is diagnosed in over one million Americans each year (American Cancer Society). This entry provides an overview of the biomedical, psychological, and socio-environmental aspects of cancer. By way of introduction, data on cancer incidence, death rates, and gender differences are provided. The overview focuses on important health psychology issues, with research findings organized by the different phases of the cancer experience, from prevention through diagnosis and treatment to long-term survival and terminal illness. Psychological interventions with demonstrated effectiveness for treating cancer patients are highlighted in each section. The conclusion provides a brief summary and discusses research directions for the 21st century.
Cancer Incidence, Death Rates, and Gender Differences
The risk of developing cancer over the course of a lifetime is 1 in 2 for men and 1 in 3 for women. Cancer is the second leading cause of death, with the number of deaths exceeded only by those from heart disease. Eighty percent of all cancer diagnoses are made in people over the age of 55 years. Table 1 displays data from the United States on the incidence and death rates by specific types of cancer diagnoses and gender. These data indicate, for example, that women are most commonly diagnosed with breast cancer and men with prostate cancer, but that lung cancer is the number one cause of cancer-related death for both genders.
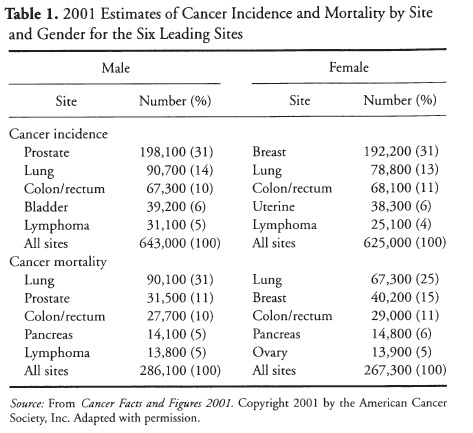 Table 1. 2001 Estimates of Cancer Incidence and Mortality by Site and Gender for the Six Leading Sites
Table 1. 2001 Estimates of Cancer Incidence and Mortality by Site and Gender for the Six Leading Sites
Biomedical, Psychological, and Socioenvironmental Issues in Cancer
Prevention
Lifestyle behaviors such as tobacco use, poor dietary habits, physical inactivity, and alcohol consumption account for an estimated 68 percent of all cancer deaths in the United States. Therefore, cancer incidence and premature death can be diminished through changes in lifestyle. Prevention efforts focus on reducing the probability of cancer onset by decreasing toxic exposures (e.g., asbestos) and providing information on risk factors (e.g., warning labels on tobacco products). Besides tobacco use, other lifestyle behaviors linked to increased cancer risk, such as dietary habits and amount of sun exposure, are targets of intervention. Diet modification, particularly reductions in fat intake and increases in fiber, are emphasized in the prevention of colorectal cancers, whereas increased avoidance of the sun and use of sun block are important in skin cancer prevention. Other prevention efforts are used to identify cancer in its earliest and often asymptomatic stages (e.g., mammography, prostate and colorectal screening). Lower socioeconomic status, lack of insurance, and rural residence can hinder awareness and access to prevention and screening interventions.
Symptom Appearance
In view of the magnitude of the cancer problem and the potential for life threat, delay in seeking medical treatment for symptoms is a surprisingly common occurrence. Whether the time lag occurs when seeing a physician for symptoms, being diagnosed, or beginning treatment, all individuals, and even some physicians, can be “delayers.” Most delay occurs in deciding whether to seek medical attention for physical symptoms (e.g., pain, loss of appetite, bleeding). Unfortunately, the development and appearance of cancer symptoms can occur over months or even years, extending delay, unlike the presentation of other serious medical problems (e.g., heart attack). Although cancer is a life-threatening disease, it is a low probability one for many individuals. Thus, delay may lengthen as people think it unlikely that their symptoms indicate a condition as serious as cancer. Economic factors such as cost of medical care, social factors such as family influence and support, personal health beliefs, and an avoidant coping style can also influence the length of delay. Barbara Andersen and colleagues have developed a model to identify factors related to medical delay (Andersen, 1992, 2002; Andersen et al., 1994, 1995). Prevention/screening efforts and shortening the delay in seeking medical care for symptoms are linked to improved survival rates for many cancers (e.g., cancers of the cervix, breast, colon, and prostate).
Diagnosis
Cancer is one of the most stressful medical diagnoses a person can receive and is accompanied by high levels of emotional distress (Weisman & Worden 1976). Depressive symptoms are the most common emotional symptoms reported by cancer patients, although anxiety symptoms are reported as well. The average rate of depression for cancer patients is 24 percent, a rate consistendy higher than rates for patients with other medical diagnoses. It is not uncommon for psychological symptoms in cancer patients to wax and wane over time, with initial adjustment difficulties developing into depressive or anxiety disorders. This situation is of particular importance because psychological symptoms are not only associated with lower quality of life but may lead to other difficulties such as poorer treatment adherence.
Importantly, the emotional problems of diagnostic-related distress are alleviated through psychological interventions (Andersen, 1992). The most effective interventions focus on stress reduction via relaxation training. Other common intervention strategies include a focus on health education, problem-solving skills, and group support. Improvements in mood, specifically stress reduction, and enhanced coping, including the use of active-behavioral strategies, can be achieved with brief, cost-effective interventions (i.e., group meetings occurring over several weeks or months).
Treatment
Some of the emotional distress occurring at diagnosis is due to the anticipation of treatment. Standard cancer therapies include any combination of surgery, radiation, chemotherapy, hormonal therapy (e.g., tamoxifen), and immunotherapy. Most treatments are preceded or followed by physical examinations, body scans (e.g., x-rays), and laboratory tests (e.g., blood tests). Thus, getting cancer treatment often represents multiple stressors for patients. What may distinguish cancer patients undergoing surgery from noncancer surgical patients are higher overall levels of presurgery distress and slower rates of emotional recovery. The scenario for radiation and chemotherapy patients is similar, but because these treatments can be lengthy (weeks or months), heightened anxiety often occurs when treatments end. At this time patients can feel “on their own” and as if they are playing a “waiting game” for cancer recurrence.
Psychological interventions to reduce patients’ treatment anxiety are frequently incorporated into routine medical care. Such efforts include procedural information (e.g., how surgery or radiation is done), information on the actual physical sensations that can be produced by treatments, and instruction in relaxation and hypnosis. These interventions produce many benefits including reduced emotional distress, decreased pain medication use and length of hospital stay, and decreased overall recovery time (e.g., amount of time until patients return to work and social activities).
Psychological intervention efforts have focused on alleviating three common treatment-related complications— adherence, fatigue, and appetite and weight changes. Adherence with treatment is important, because the expectation and experience of unpleasant side effects such as fatigue and nausea/vomiting not only diminish patients’ quality of life, but can also be so discouraging or annoying that a patient may be reluctant to continue treatment. Nonadherence with treatment has also been related to emotional distress, lower income, and age (e.g., adolescent patients). It is a behavioral problem that can directly affect the effectiveness of cancer therapy. For instance, when patients do not adhere to medical recommendations, treatment dosage may be reduced, which can, in turn, lower the cure rate. Psychological interventions to improve patient adherence focus on a variety of techniques, including appointment and medication reminders, clearly written and specific treatment communications, and home visits. Additionally, preparatory hospital-based interventions such as offering a tour of the oncology clinic, videotape presentations about treatment, discussion/question sessions, and take-home information are especially effective in improving coping with treatment.
Fatigue is the most common symptom reported following treatment, especially by cancer patients receiving radiation or chemotherapy. Importantly, fatigue is distinct from depression. Symptoms of fatigue (e.g., feeling tired, a lack of energy, sleepy, confused) have been related to decreased quality of life, reduced overall daily functioning, and poor treatment adherence. Psychological interventions focus on increasing tolerance to fatigue in a number of ways: (1) providing information on side effects and activity/rest cycle recommendations (e.g., naps in the afternoon), (2) increasing physical activity (e.g., walking, flexibility, or strengthening exercises), (3) enhancing coping efforts (e.g., planning and scheduling activities, decreasing nonessential activities, reliance on others for assistance), and (4) improving nutritional status (e.g., protein intake).
Appetite and weight changes are also significant problems for cancer patients. Malnutrition is associated with increased morbidity and mortality. Food aversions learned in connection with chemotherapy are rapidly acquired (usually after one to three treatments) and although these aversions may not involve appetite or weight loss, patients may unknowingly develop aversions to their favorite foods. These aversions can affect patients’ daily routine and perceived quality of life. Since the late 1980s, research has revealed that many cancer patients will develop nausea and/or vomiting in response to chemotherapy treatments (Carey & Burish, 1988). However, anti-nausea/vomiting drug treatments have dramatically reduced the incidence of such problems. Psychological treatments for these problems include hypnosis, progressive muscle relaxation with guided imagery, systematic desensitization, cognitive distraction, and biofeedback. Effective preventive care also reduces the likelihood of conditioned anticipatory reactions (i.e., nausea and vomiting associated with previously neutral events such as going to the hospital and sitting in the waiting room). Weight gain resulting from chemotherapy or hormonal treatments is an important issue for women with cancer and appears to be a risk factor for breast cancer recurrence. Behavioral weight management interventions teach healthy eating habits (e.g., reducing daily fat intake and increasing fiber) and promote exercise to maintain or lose weight.
Recovery and Survivorship
The term “survivor” typically refers to individuals who have survived cancer at least 5 years, as the probability of recurrence declines significantly after that time for most cancers. As the prognoses for many cancer diagnoses have improved, there is increased attention to quality of life, particularly for long-term survivors of cancer. Studies suggest that by 1 year following treatment the severe distress of diagnosis and treatment declines and emotions stabilize. Emotional difficulties, therefore, do not persist for the majority of cancer survivors. In fact, many survivors report positive life changes (e.g., greater empathy and appreciation for life, closer relationships, living life more fully in the present moment). Still, many cancer survivors do report specific problems beyond treatment including premature menopause, sexual disruptions, financial concerns, and fears of recurrence.
Premature or abrupt menopause is a difficult circumstance for many women receiving chemotherapy, and occurs more frequently in older women or women receiving higher doses of chemotherapy. The consequences of chemotherapy-induced menopause include sleep disturbances, hot flashes, mood swings, difficulties with vaginal lubrication, cessation of menses, and infertility. These symptoms may be even more severe than those experienced during naturally occurring menopause. In addition, for young women, fertility concerns can have a major impact on quality of life. Issues related to premature menopause and infertility should be discussed early and often to promote coping and adjustment during survivorship.
Sexuality is also disrupted for many cancer survivors. All patients with solid tumors (85 percent) and many treated for blood-related cancers (e.g., lymphoma and leukemia) are vulnerable to sexual dysfunction (e.g., desire and arousal problems and painful intercourse). Estimates of cancer-related sexual dysfunction range from 10 to 20 percent for breast cancer patients treated with lumpectomy to 100 percent for men having surgical prostate removal. Disease and treatment side effects are the primary cause of sexual problems. Feelings related to perceived attractiveness and body image changes associated with treatment (e.g., facial or genital surgery, loss of hair due to chemotherapy) may also play a role in sexual dysfunction. If sexual problems do develop, they usually do so when intercourse resumes, and, if untreated, are unlikely to resolve. Several psychological interventions facilitate sexual adjustment including (1) consideration of the optimal timing for sexual activity (e.g., when fatigue is at its lowest), (2) use of strategies to facilitate desire (e.g., fantasy and erotic materials), (3) expanding the behavioral repertoire (e.g., sexual activities in lieu of intercourse and alternative intercourse positions), and (4) use of lubricants to counter vaginal dryness. Interventions to enhance couples’ sexual communication or rehearse sharing information about cancer with a prospective partner are also beneficial.
Other difficulties experienced by cancer survivors include financial disruption and fears of recurrence. Cancer treatments are expensive and occupationally disruptive. Some cancer survivors report chronic economic stress including increased insurance premiums, loss of insurance, and income reductions due to work absences. In addition, the majority of survivors report ongoing concerns about cancer recurrence that are exacerbated during subsequent medical appointments. Psychological interventions during this phase of the cancer experience include referrals for potential financial and insurance assistance, open discussion of concerns regarding potential recurrence, and relaxation training to reduce stress at follow-up medical appointments.
Recurrence and Metastatic Cancer
Many patients experience a rebound in emotional distress when cancer recurs, with as many as 45 percent reporting symptoms of anxiety or depression at the time of recurrence diagnosis. Persons experiencing a greater number of current stressors, particularly financial difficulties, have an elevated risk of emotional distress during recurrence. Younger patients and patients with greater pain or discomfort and less hopefulness also report greater distress. In addition, partners or spouses may be more distressed by a recurrence diagnosis than the initial cancer diagnosis, and may become more distressed than the cancer patient. The partner or spouse plays an essential role in supporting the patient through this difficult experience. However, many couples are reluctant to discuss the meaning of the recurrence and fears of loss. Psychological interventions designed to improve couple communication can be useful to address these concerns. Supportive-emotionally expressive group interventions and problem-solving approaches also bring about important emotional benefits such as decreased distress, enhanced coping, and improved self-esteem.
Two of the most distressing aspects of metastatic cancer are pain and delirium. Pain is more common and less controllable for individuals with metastatic cancer (i.e., disease that has spread from the original site). Eighty percent of patients with metastatic cancer report moderate to severe pain as compared to 40 percent of earlier-stage patients. The major cause of cancer pain is direct tumor involvement (e.g., metastases to bone and nerve compression), but pain can also be the result of treatment (e.g., surgery and radiation). If pain worsens or is difficult to control, daily functioning can be impaired, social interactions may suffer, and quality of life may deteriorate. Pain is associated with depression and anxiety and inadequately controlled pain has been cited as a primary reason for requests for physician-assisted suicide. In addition to pain-controlling medications, psychological interventions for advanced cancer pain benefit both patients and family members. Interventions include dispelling myths about addiction to pain medication, teaching self-control techniques such as hypnosis and relaxation, and offering education regarding early identification of pain symptoms and assertive communication leading to more effective pain control.
Another frequent complication of metastatic cancer is delirium. Approximately 75 percent of patients with metastatic cancer meet criteria for delirium as compared to 8 percent of patients during other illness phases. Delirium is characterized by problems with awareness, attention, and memory. Individuals with delirium may also be restless and disoriented, which is distressing to family members and caregivers. Delirium in cancer patients is caused by a number of factors including chemotherapy, narcotics used for pain control, and brain metastases. Although delirium is a reversible brain disorder, it is often misunderstood and misdiagnosed, with symptoms often attributed to depression and anxiety. Psychological interventions aimed at the early identification of symptoms and helping patients and caregivers understand the transient nature of delirium can reduce anxiety and create immediate emotional benefits. Organization of the patients environment to include calendars, clocks, and objects of personal significance also helps to orient the patient to the date, time, and location.
Terminal Cancer
Cancer is considered terminal when the disease is no longer responsive to treatment. At this point, the focus is on palliative care. The World Health Organization (1990) defines palliative care as “the active total care of patients… including control of pain, of other symptoms, and of psychological, social, and spiritual problems. The goal of palliative care is achievement of the best possible quality of life for patients and their families.” The most common physical symptoms of terminal cancer include pain, difficulty breathing, fever, nausea or vomiting, constipation or diarrhea, loss of appetite, and weight loss. Up to 60 percent of individuals with terminal cancer also experience psychological difficulties including adjustment disorders, depression, anxiety, and delirium. At this phase of illness, patients report distress associated with unmanaged physical symptoms, inability to carry on meaningful activities, and insufficient emotional support, especially for the unmarried or those living alone. During terminal illness many individuals seek emotional support related to their worries or fears. These fears are often existential in nature (e.g., concerning the meaning of life and death), or more pragmatic, related to the families’ ability to carry on beyond the death of the patient.
The terminal phase is especially difficult for family members. Many family members experience a period of anticipatory grieving that involves physical or emotional distancing from patient suffering as a means of managing the eventual death of the loved one. Some caregivers have chronic health problems of their own that can be exacerbated by exhaustion or sleep deprivation. Many caregivers also suffer significant reductions of income due to work absenteeism resulting in financial distress. Family members report needs for assistance to assure the patient’s comfort, frequent information regarding the patient’s condition, needs for the support of other family members, and acceptance and support from health care professionals. Psychological interventions that focus on the quality, not quantity, of survival are important when death is inevitable. These efforts emphasize patient control over the environment, attention to unfinished family business, and continued involvement in feasible, but meaningful activities. Listening to patients’ reminiscences, helping them develop meaning, and offering support to struggling family members are important in enhancing quality of life during terminal illness.
Summary and Conclusions
Psychological interventions are a valuable addition to medical treatment across all phases of the cancer experience, from efforts to enhance health-promoting behaviors and consequently prevent cancer, to efforts to facilitate meaning in the face of terminal disease. Psychological interventions have an established impact on symptom management (i.e., nausea and vomiting, fatigue, pain control), stress reduction, mood improvement, and overall quality of life. Psychological interventions may also improve treatment adherence and facilitate healthy lifestyle changes (e.g., diet and exercise), although maintenance of these changes is challenging for many patients.
Since the late 1980s, research efforts have also focused on the effect of psychological interventions on immune functioning and survival. A study published by David Spiegel and colleagues at Stanford University in 1989 reported an 18-month survival benefit for women with metastatic breast cancer who participated in a year-long supportive-emotionally expressive therapy group. However, the studies published since Spiegel’s original work report inconsistent results. A biobehavioral model of cancer stress and disease course has also been developed to describe the mechanisms by which the stress could influence survival. Thus far, significant progress has been made in understanding the biomedical, psychological, and socioenvironmental aspects of cancer. Psychological interventions are known to improve quality of life from diagnosis to terminal illness, regardless of the duration of the cancer experience.
Leave a Reply