Introduction
The health belief model (HBM) emerged from the work of U.S. public health researchers Godfrey Hochbaum, Stephen Kegels, Howard Leventhal, and Irwin Rosenstock, who were attempting to develop models to explain why individuals fail to engage in preventive health measures. Early studies by Hochbaum concerned why people seek diagnostic x-rays for tuberculosis. In 1956 Hochbaum published a paper on this topic, which contained references to factors that would later become part of the HBM, such as perceived personal susceptibility and perceived benefits of engaging in the preventative behavior. The first clear formulation of the HBM appeared in a paper by Rosenstock in 1966, and was later refined by Marshall Becker in 1974. Today, the HBM is one of the most widely used social cognition models in health psychology. This entry describes the model, defines the various components within the model, and summarizes how the HBM has been used to predict and explain health behaviors. Finally, ways in which the HBM has been used to help design health interventions are discussed.
Components of the Health Belief Model
The model contains two main components, (1) perceptions of the threat of illness and (2) evaluations of the effectiveness of behaviors aimed at counteracting the threat of illness (see Figure 1). Threat perceptions result from beliefs about the perceived susceptibility to the illness and the perceived severity of the consequences of the illness. Perceived susceptibility refers to an individuals assessment of his or her personal risk of contracting a condition. Perceived severity is concerned not just with medical consequences, but also with the potential effects of an illness on an individual’s job, family life, and social relations. Whether an individual engages in a health-related behavior is determined by the combined effect of these two variables. An individual will decide on the particular action to be taken by evaluating the possible alternatives. Health behaviors will be evaluated in terms of their perceived benefits or efficacy and also by their perceived costs or barriers. Examples of perceived benefits are the reduction of susceptibility to an illness or the reduced severity of an illness. Examples of perceived barriers are the health behavior being painful, inconvenient, unpleasant, or expensive. Therefore, according to the HBM, individuals are likely to follow a particular health action if they believe that they are susceptible to a particular condition or illness that they consider to be serious, and believe the benefits of the action taken to counteract the condition or illness outweigh the costs.
Although Hochbaum discussed cues to action in some of his early publications, they were not added to the HBM until later. Health motivation was also not an original part of the model, but in 1974 Becker published an influential paper suggesting that it should be added to the model. According to Janz and Becker (1984), cues to action include a diverse range of triggers to the individual taking action and are commonly divided into factors that are internal (e.g., physical symptom) or external (e.g., mass media campaign, advice from others such as physicians) to the individual. Becker defined health motivation as readiness to be concerned about health matters and argued for its inclusion in the model as certain individuals may be predisposed to respond to cues to action because of the value they place on their health.
Other influences on the performance of health behaviors include demographic factors such as age, gender, ethnicity, socioeconomic status, and education. Psychological characteristics such as personality, peer pressure, and perceived control over behavior are also thought to play a role. Both these groups of factors are assumed to exert their influence indirectly by influencing the other six components of the HBM. Evidence, however, to support this contention is mixed. For example, a study by Orbell et al. (1996) found that HBM components did mediate the effects of social class on uptake of cervical screening, but did not mediate the effects of marital status or sexual experience.
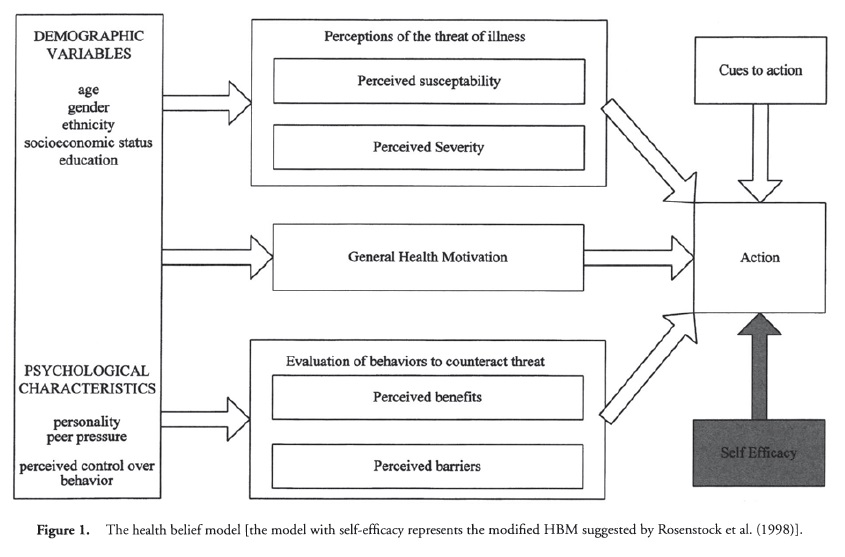 Figure 1. The health belief model [the model with self-efficacy represents the modified HBM suggested by Rosenstock et al. (1998)].
Figure 1. The health belief model [the model with self-efficacy represents the modified HBM suggested by Rosenstock et al. (1998)].
Applications of the Health Belief Model
The HBM has been applied to a wide range of populations and health behaviors. Sheeran and Abraham (1996) distinguished three broad areas of research: (1) preventative health behaviors, (2) sick role behaviors, and (3) clinic use. They noted that the preventative health behaviors to which the HBM have been applied include smoking, alcohol use, diet, exercise, genetic screening, health screening, vaccination, breast self-examination, contraceptive use, and dental behaviors. Sick role behaviors include compliance with professionally recommended medical regimens in response to illness. Sheeran and Abraham described how the HBM has been used to study adherence to a wide range of regimens such as those concerned with hypertension, diabetes, and renal disease. Examples of how the HBM has been applied to clinic use include physician visits for preventative, psychiatric, and parent and child conditions. According to Sheeran and Abraham, there is no strong evidence that the HBM has been more predictive of behavior in any one of these areas compared to any other.
The HBM has also been used to inform health interventions. For example Willamson and Wardle (2002) employed the HBM when designing an intervention aimed at increasing participation with colorectal cancer screening. The study placed particular emphasis on seven barriers that have been identified with respect to colorectal cancer screening. The barriers were presented in a series of cartoons that also offered solutions to the barriers and provided professional advice. Other such interventions include that by Gilliam et al. (2001), who drew upon the HBM when designing a HIV prevention program for adolescents. Such interventions have reported reasonable levels of success in changing behavior, demonstrating the practical utility of the model.
Effectiveness of the Health Belief Model
In 1984 Janz and Becker carried out a review of research that had employed the HBM. They reviewed 46 studies and found that in 89 percent of them, the barriers component had a significant relationship with health behavior, susceptibility was significant in 81 percent of the studies, benefits in 78 percent, and severity in 65 percent. A later study by Harrison et al. (1992) went a step further and examined the strength of the relationships between the constructs. These researchers identified 234 studies that had employed the HBM, although only 16 of these were found to measure each of the components adequately. In line with Janz and Becker, Harrison and his colleagues found that the barriers component had the highest average correlation with health behavior (r = —0.21), followed by the susceptibility (r = 0.15), benefits (r = 0.13), and severity (r = 0.08) components. Although the predictive power of individual components is relatively modest (each only accounts for between 0.5 and 4 percent of variance in behavior), it is the combined effects of the six health beliefs that is generally of interest.
Criticisms of the Health Belief Model
Despite the popularity of the HBM, it suffers from a number of weaknesses compared to other similar social cognition models. The manner in which the variables within the model combine to produce behavior has not been precisely specified and this has resulted in the HBM being frequently tested as six independent predictors of behavior. There are also frequent variations in the manner in which the six constructs are employed. Important social cognitive variables found to be highly predictive of behavior in other models are not incorporated in the HBM. For example, social pressure and intentions to perform a behavior are key components of the theory of reasoned action and theory of planned behavior but do not appear in the HBM. Self-efficacy (i.e., an individuals belief that he or she is capable of performing a specific behavior to attain a desired outcome) is also a powerful predictor of behavior in models based on social cognitive theory but were not originally included in the HBM. Rosenstock et al. (1988) have, however, since published a paper that incorporates self-efficacy into the model.
The HBM does not specify a causal ordering among the variables, as is done in other models. Such information might allow for more powerful analysis of data and clearer indications of how interventions may have their effects. It is possible that threat is better viewed as a more distal predictor of behavior. The model also does not distinguish between a motivational stage dominated by cognitive variables and a volitional phase where action is planned, performed, or maintained. Such distinctions are thought to be important in understanding various health behaviors. There is clearly much scope for the model to be refined and improved upon.
In summary, the HBM has been very widely used and provides a useful framework for examining health behaviors and identifying key health beliefs. It has met with moderate success in predicting a range of health behaviors. One appealing characteristic of the HBM is that it was developed by public health researchers working directly with health behaviors. This has resulted in the model containing constructs that possess face validity to those working in the health promotion and disease prevention areas. The models popularity may in part be due the commonsense operationalization of a number of relevant cognitive variables.
Leave a Reply