 Calcium
Calcium
For most of human history, people got their calcium from plants, primarily wild, leafy greens. Dairy foods didn’t become part of the human diet until around 10,000 years ago and even then they were consumed only in some parts of the world. Calcium-rich greens were so abundant in early diets that some nutritional anthropologists speculate that people consumed as much as 3,000 milligrams per day of calcium from these foods, or about three times our current recommended in-takes. The cultivated greens that are available to vegans today are lower in calcium than the wild vegetables available to our ancestors, but they can still make a significant contribution to calcium intake. Vegans can also get calcium from some legumes and nuts, and from fortified foods.
There is no question about whether vegan diets can provide enough calcium. They can. But that doesn’t mean that they do. In studies of vegans, average calcium intakes often fall well below recommendations. One unanswered question has to do with calcium needs of people who eat plant-based diets. Do vegans need less calcium? You’ll see that it’s not so easy to figure this out.
Calcium and Bones
While bones might seem solid and static, they are actually quite dynamic. The skeleton acts as calcium storage, providing a steady supply of calcium to the blood where it is needed for muscle relaxation, nerve cell transmission, and a host of other functions. Some of this calcium is regularly lost in the urine and must be replaced by dietary sources. As a result, bones are in motion—breaking down to release calcium to the blood and then taking up new calcium and rebuilding. Getting enough calcium is important for bone health, but reducing the amount that is lost through the urine could be important too.
Bones grow through the first three decades of life, becoming longer, heavier, and denser. By their late twenties or early thirties, most people have achieved peak bone mass, and their skeleton is as heavy and dense as it is going to get. There is some evidence that peak bone mass determines bone health and risk for osteoporosis in later years.
Beginning at age forty-five or so, there is a shift in metabolism and bone mass begins to decline. Efforts to slow calcium losses from the body and provide enough calcium to keep bones strong are important for preventing osteoporosis, especially for women, who can begin to lose bone rapidly after menopause.
Good bone health depends on a complex interplay of factors that affect both absorption of calcium and calcium losses from the body. Diet, lifestyle, and genetics all play a part in calcium balance. Figuring out how these factors interact and affect calcium needs has been an ongoing subject of debate among researchers, and some of the issues may be especially important for vegans.
The Relationship of Calcium Intake to Bone Health
Calcium is different from other nutrients in that it isn’t associated with an acute deficiency disease. With most nutrients, if your intake is too low, you’ll get sick. That’s not true for calcium because levels in the blood are very tightly controlled. Even a small change in those levels can be life-threatening, so the body utilizes stored calcium in the bone plus the filtering system of the kidneys to keep calcium concentrations within strict boundaries. You can’t ascertain calcium status by measuring blood levels of this mineral because those levels are always the same. But while a low calcium diet doesn’t cause an acute nutritional deficiency, a chronically low intake can raise the risk for osteoporosis later in life.
Osteoporosis is a crippling and debilitating disease of severe bone loss—as much as 30 to 40 percent of total bone—that affects an estimated 10 million Americans. Eighty percent of Americans with osteoporosis are women.
When nutrition scientists look at the relationship of diet to bone health, they look at both bone density and fracture rates. And the findings are anything but clear. How much calcium humans need and the extent to which varying intakes affect bone health are topics of intense research. Many large epidemiologic studies fail to show that high calcium intakes protect against bone fractures. The balance of evidence suggests, however, that calcium and vitamin D together are protective.
Protein and Calcium: More Questions than Answers
A couple of decades ago, studies of bone health among people in different countries revealed an interesting pattern. Rates of hip fracture (which is often used as a marker for bone health) were highest in countries with the highest intakes of animal protein, even though calcium intake was also high. The findings suggested that too much protein was worse for bones than too little calcium. And, in fact, there is a biological explanation to back this.
High intakes of certain proteins increase the blood’s acidity, kicking off a chain of reactions to bring blood back to a more neutral pH. A release of calcium from the bones is one part of the process. The more acidic the blood, the greater the loss of calcium from bones. Meat proteins are among the most acid-producing foods, followed by proteins from grains and dairy. Diets high in fruits and vegetables are the least acidic.
Based on this, it seems to make sense that people who eat animal protein should need more calcium to replace what is constantly being leached from their bones. Conversely, wouldn’t vegans, whose diets contain no animal proteins, have lower calcium needs? This sounds like an obvious conclusion, but it’s not quite that straightforward.
First, the studies comparing different populations have limited usefulness. These are ecological studies, and we saw in Chapter 1 that they provide only weak evidence. There are just too many cultural and genetic variations among people of Asian, African, and Caucasian backgrounds for us to make direct comparisons about their protein intakes and bone health. For example, people of African descent have a genetic predisposition toward stronger, heavier bones. And a slight genetic advantage in hip anatomy among Asians protects against fracture.
There are cultural differences too. Asians tend to have better balance, so they are less likely to fall and break a bone. And in some cultures, elderly people rarely leave their home without a younger family member at their side and are therefore less likely to fall. In fact, while Asian populations fare well in comparisons of hip-fracture rates, their spinal bone health is similar to westerners’. This suggests that there is something in their genes or lifestyle that is specifically protective against hip fracture but doesn’t affect other parts of the skeleton. If diet were the protective factor, the benefits would show up in all parts of the skeleton.
As a result, these cross-cultural studies might tell us more about culture and genetics than about diet, which means that these comparisons don’t tell us a whole lot about how much calcium western vegans might need.
It’s better to look at clinical research, where the effects of protein are directly observed and measured. Findings from clinical studies show the following:
- Consuming isolated animal proteins—that is, just the pure protein portion of a food—has a direct and significant effect on calcium losses, but that effect is often lost when subjects are fed whole, high-protein foods. The reason may be that other factors in foods, like phosphorus, counteract the urinary losses.
- While protein can increase calcium losses, it also enhances calcium absorption from foods. There is evidence that these positive effects on absorption may outweigh or at least compensate for the negative effects of calcium loss.
- In some studies, higher protein intake is actually associated with better bone health, and protein supplements can help bone fractures heal more quickly.
The evidence suggests that effects of protein on bone health may be dependent on how much calcium is in your diet. That is, protein is beneficial in people who consume more calcium. In addition to the positive effects of protein on calcium absorption, high-protein diets improve muscle mass, which is associated with better bone health. And protein also boosts levels of compounds that may stimulate bone formation.
If all of this leaves you feeling confused, you aren’t alone. The complete story about protein and calcium balance is still unfolding. But based on what we know right now, it is far too simplistic to say that vegans have lower calcium needs than omnivores or that restricting protein intake improves bone health. The science of calcium, protein, and bone health is too complex and the research too conflicting to justify those conclusions.
Vegan Diets and Bone Health
Unfortunately, a number of resources for vegans in books and online suggest that calcium requirements are lower for those on plant-based diets, and it is possible that this has not served vegans well. While we don’t have much information about bone health in vegans, the few available studies suggest that some vegans don’t get enough calcium. In the studies that show vegan bone health to be worse than in omnivores, it is due very simply to lower calcium intakes. So far, only one study has looked at actual risk for fracture; it found that vegans had a higher chance of breaking a bone than non-vegans—but when they consumed enough calcium, their risk of fractures was the same as in omnivores.
So where does this leave us in terms of calcium requirements? Given all of the inconsistencies in the research and the findings, limited as they are, about bone health in vegans, we recommend that vegans meet the calcium recommendations that have been established for the general population.
Recommendations for daily calcium intake for western populations range from 700 milligrams in the United Kingdom to 1,000 milligrams in the United States. The U.S. recommendation is an AI, which you may remember from Chapter 1 is a “best guess” kind of recommendation. There is evidence to suggest that 700 milligrams may meet the needs of most people, but it also may not be enough for everyone. Calcium needs can vary considerably among individuals, primarily because there is a big genetic variation in absorption rates. Aiming for the U.S. recommendation of 1,000 milligrams for adults can provide good insurance.
Calcium without Milk?
Getting calcium from plants might seem a little strange in a society that is so focused on dairy foods as a source of calcium. But some research suggests that even omnivores get as much as 40 percent of their calcium from plant foods. And really, why should that be surprising? Omnivores eat broccoli, baked beans, hummus, and other plant foods that are good sources of calcium.
While a strong dairy lobby has convinced many consumers that milk and other dairy foods are essential for a healthy diet, the ability to drink milk into adulthood is not the norm throughout the world. Normal development throughout most of the world involves a gradual loss of the enzyme needed to digest milk sugar after children are weaned from breast milk. Indications are that a mutation occurred some ten centuries ago among northern Europeans that resulted in the continued production of this enzyme, allowing that population to drink milk into adulthood.
In the United States, we refer to the lack of this enzyme as “lactose intolerance.” But that’s definitely a western bias since this “intolerance” is not a lack or an abnormality; it’s part of normal human development in most people. Since many people the world over need to meet calcium needs without dairy foods, there is no reason why vegans can’t do it as well. And with our access to a wide variety of calcium-rich and fortified foods, it’s not at all difficult.
Meeting Calcium Needs on a Vegan Diet
The amount of any nutrient in a food is not equal to the amount that actually makes its way from the intestines into the bloodstream. The bioavailability of a nutrient from a particular food refers to the amount of that nutrient that is likely to be absorbed and used, and it’s affected by a number of factors.
A few leafy green vegetables—spinach, beet greens, Swiss chard, and rhubarb—are high in naturally occurring compounds called oxalates that bind calcium and make it essentially unavailable to the body. But the availability of calcium from low-oxalate vegetables—kale, col-lards, broccoli, and turnip greens—can be as high as 50 percent.16 Calcium absorption from soyfoods, like calcium-set tofu (tofu that is processed with calcium-sulfate) and fortified soymilk, is around 25 to 30 percent, which is about the same as from cow’s milk. Calcium absorption from nuts and legumes is somewhat lower, around 20 percent.
The recommended intake of 1,000 milligrams of calcium is based on the assumption that most people absorb around 30 percent of the calcium in their diet. If you’re eating a varied diet that includes several different types of calcium sources, including leafy greens and soy products, you don’t need to worry that some of the calcium from other foods is absorbed less efficiently.
It’s possible to get plenty of calcium just from eating foods that are naturally rich in this mineral, but it does take some effort. (This is equally true for people who consume dairy foods, since many people who drink milk don’t meet calcium requirements. That’s why so many products on the market—from cereals to juices to protein bars—are fortified with calcium.) Using fortified foods like juices and nondairy milks can make it easier to meet calcium recommendations on a vegan diet.
It’s also helpful to pay attention to the effects of processing. For example, frozen leafy greens are higher in calcium than fresh, although this is simply because their volume tends to be more concentrated. Processing also affects the amount of calcium in different types of tofu. Tofu production involves ingredients that cause soymilk to curdle. The two most common—often used together—are magnesium-chloride (nigari in Japanese) and calcium-sulfate. When calcium-sulfate is used, tofu is often an excellent source of calcium. Also, firm tofu tends to have a higher calcium content than soft. It’s important to read package labels, though, since the amount of calcium in different brands and different types of tofu varies widely.
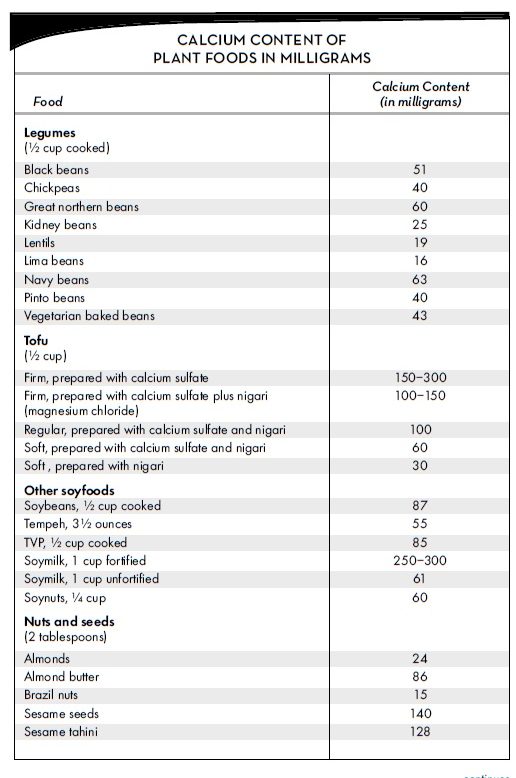
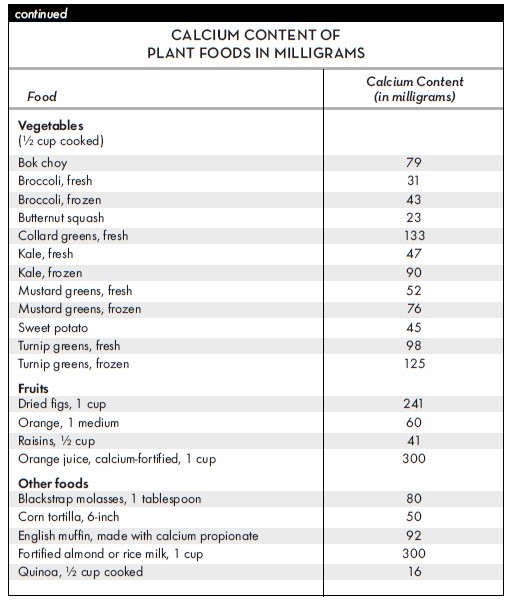
In the Vegan Food Guide in Chapter 7, we recommend 6 to 8 servings of calcium-rich foods per day. This allows you to mix and match small servings of a variety of calcium-rich foods or get all of your calcium from larger amounts of just a few foods. One serving is V cup fortified plant milk or juice, V cup cooked, calcium-rich vegetables, V cup tofu or tempeh, 2 tablespoons almond butter or tahini, lA cup soynuts, or V cup dried figs. The table on page 45 shows calcium contents of a wide variety of plant foods.
Tips for Getting Enough Calcium
- Follow the recommendations in the Vegan Food Guide in Chapter 7.
- If you use calcium-fortified soymilk, give the carton a good shake before pouring since the calcium can settle to the bottom.
- Look for calcium-set tofu, which is tofu that includes calcium-sulfate as an ingredient.
- Learn to love greens! The ones that are low in oxalates— collards, kale, turnip, and mustard greens—are good sources of well-absorbed calcium as well as other nutrients that are important for bone health.
- Make your own trail mix using soynuts, almonds, and chopped figs and keep it on hand for snacks.
- Choose calcium-fortified brands when you drink fruit juices.
- If your intake falls short, make up the difference with a supplement.
Vitamin D
Adequate vitamin D is every bit as important as calcium for maintaining bone health. But is vitamin D a nutrient? Not exactly, since we can make all we need when our skin is exposed to ultraviolet rays from sunlight. In fact, for most of human history, this is where people got their vitamin D since it occurs naturally in very few foods. But as people moved away from the equatorial zones and began to spend more time indoors, vitamin D deficiency became a problem. In the early 1900s, rickets (soft bones that don’t develop well in children) was a significant public health problem that led to fortification of cow’s milk with vitamin D.
While the focus has long been on bone health, more recent research suggests that suboptimal vitamin D levels are linked to fibro-myalgia, rheumatoid arthritis, multiple sclerosis, depression, muscle weakness, diabetes, hypertension, and cancer. The current AI for vitamin D in adults is 600 IUs (vitamin D is also measured in micrograms; 1 microgram equals 40 IUs). But many experts believe that it may take as much as 1,000 IUs or 25 micrograms to maintain ideal blood levels of vitamin D.17 While this continues to be a controversial area, we favor the higher recommendation.
Dietary Sources of Vitamin D
The only significant, natural sources of vitamin D in foods are fatty fish, eggs from chickens who have been fed vitamin D, and mushrooms treated with ultraviolet rays. Many people think that milk is a good natural source of vitamin D, but it isn’t. Milk contains no vitamin D unless it has been fortified and is no more natural a source of this vitamin than any other fortified food.
There are two types of vitamin D used in fortified foods and supplements. Vitamin D3 or cholecalciferol is derived from animals, usually from sheep’s wool or fish oil. Vitamin D2 or ergocalciferol is usually obtained from yeast and is vegan. The evidence suggests that the two types are absorbed equally as well but that blood levels of vitamin D2 decline more quickly when megadoses of the vitamin are consumed. At the smaller dose that we recommend—1,000 milligrams per day—vitamin D2 appears to be as effective as vitamin D3.
Getting Enough Vitamin D for Optimal Health
Concern about skin cancer has people using powerful sunscreen or shying away from sun exposure altogether. However, in addition to blocking the harmful effects of the UV light on the skin, sunscreen blocks vitamin D synthesis. And there are plenty of other factors that affect vitamin D synthesis in the skin. Older people need longer exposure and so do people with dark skin. Smog can interfere with vitamin D synthesis and the farther away you are from the equator, the more sun exposure you need to make vitamin D. Some research suggests that Americans living in the northern part of the country do not make any vitamin D during the winter months.
To make adequate vitamin D for one day, a light-skinned person needs ten to fifteen minutes of midday (10:00 a.m. to 2:00 p.m.) sun exposure, without sunscreen, on a day when sunburn is possible. Dark-skinned people need twenty minutes and older people need thirty minutes.
If your sun exposure doesn’t match these guidelines, then you need to take a supplement or use fortified foods. We recommend 25 micrograms (1,000 IU) per day of vitamin D2.
Many foods, including most breakfast cereals, are fortified with vitamin D. Almost all use vitamin D3, which is derived from animals. Most brands of fortified soymilk and other nondairy milks use vitamin D2, which comes from yeast exposed to UV rays.
For food labeling purposes, the Daily Value for vitamin D is 10 micrograms (400 IU). So if a food provides 25 percent of the Daily Value for vitamin D, it contains 2.5 micrograms (100 IU) of vitamin D per serving. Vitamin D-fortified soy, almond, hemp, or rice milk normally has 2 to 3 micrograms (80 to 120 IU) per cup. You can see from these numbers that it’s not that easy to meet the recommended 1,000 IU per day from fortified foods. If your sun exposure isn’t adequate, you will probably need to use a vitamin D supplement. Most natural foods stores carry supplements of plant-derived vitamin D2, or you can order one from the online sources in the resource section of this book.
Bone Health: More than Calcium and Vitamin D
Calcium and vitamin D have well-deserved reputations as bone-strengthening nutrients, but they don’t act alone. The following are all important for protecting bone health.
- Stay physically active. Exercise is absolutely crucial to bone density and strength; it’s probably the single most important factor in preventing bone loss. Choose weight-bearing and high-impact exercise to get the greatest benefit, such as weight-lifting, jogging, and step aerobics. Biking and swimming are not especially valuable to strengthening bones.
- Maintain a healthy weight and by this, we mean don’t let your weight get too low. When it comes to bone health, being a few pounds above your ideal weight is better than being a few pounds below it. Rapid weight loss is associated with bone loss, so if you have some pounds to shed, aim for a slow reduction while building more muscle and protecting bones through exercise.
- Eat plenty of fruits and vegetables because they keep the blood more alkaline. In fact, some researchers have suggested that the best diet for maintaining healthy bones is one that is rich in calcium, contains plenty of protein to boost calcium absorption, and is generous in fruits and vegetables to keep the blood alkaline. But fruits and vegetables also provide nutrients that are good for bones, such as vitamin K and the minerals boron, potassium, and magnesium. Vitamin C also plays a role in bone formation and high vitamin C intake has been linked to better bone health. Plant foods are the best sources of vitamin K and potassium, and they are the only sources of vitamin C.
- Avoid excess sodium, which is linked to calcium losses. Lightly salting your food is fine, but an overdependence on processed foods can make vegan diets too high in sodium.

Leave a Reply